A scaphoid (navicular) fracture is a break in one of the small bones of the wrist. This type of fracture occurs most often after a fall onto an outstretched hand. Symptoms of a scaphoid fracture typically include pain and tenderness in the area just below the base of the thumb. These symptoms may worsen when you try to pinch or grasp something.
Treatment for a scaphoid fracture can range from casting to surgery, depending on the fracture’s severity and location on the bone. Because portions of the scaphoid have a poor blood supply—and a fracture can further disrupt the flow of blood to the bone—complications with the healing process are common.
A scaphoid fracture is usually described by its location within the bone. Most commonly, the scaphoid breaks in its mid-portion, called the “waist.” Fractures can also occur at both the proximal and distal ends of the bone.
Scaphoid fractures are classified according to the severity of displacement–or how far the pieces of bone have moved out of their normal position:
Non-displaced fracture. In this type of fracture, the bone fragments line up correctly.
Displaced fracture. In this type of fracture, the bone fragments have moved out of their normal position. There may be gaps between the pieces of bone or fragments may overlap each other.
What is the cause ?
A scaphoid fracture usually occurs when you fall onto an outstretched hand, with your weight landing on your palm. The end of the larger forearm bone (the radius) may also break in this type of fall, depending on the position of the hand on landing.
The injury can also happen during sports activities or motor vehicle collisions.
Fractures of the scaphoid occur in people of all ages, including children.There are no specific risk factors or diseases that make you more likely to experience a scaphoid fracture. Some studies have shown that using wrist guards during high-energy activities like inline skating and snowboarding can help decrease your chance of breaking a bone around the wrist.
What are the symptoms ?
Scaphoid fractures usually cause pain and swelling in the anatomic snuffbox and on the thumb side of the wrist. The pain may be severe when you move your thumb or wrist, or when you try to pinch or grasp something. Unless your wrist is deformed, it might not be obvious that your scaphoid bone is broken. With some scaphoid fractures, the pain is not severe and may be mistaken for a wrist sprain.
Pain in your wrist that does not go away within a day of injury may be a sign of a fracture—so it is important to see a doctor if your pain persists. Prompt treatment of a scaphoid fracture will help avoid potential complications.
What is the treatmemt ?
The treatment your doctor recommends will depend on a number of factors, including:
The location of the break in the bone
Whether the bone fragments are displaced
How long ago your injury occurred
Nonsurgical Treatment
Fracture near the thumb. Scaphoid fractures that are closer to the thumb (distal pole) usually heal in a matter of weeks with proper protection and restricted activity. This part of the scaphoid bone has a good blood supply, which is necessary for healing. For this type of fracture, your doctor may place your forearm and hand in a cast or a splint. The cast or splint will usually be below the elbow and include your thumb. Healing time varies from patient to patient. Your doctor will monitor your healing with periodic x-rays or other imaging studies.
Fracture near the forearm. If the scaphoid is broken in the middle of the bone (waist) or closer to the forearm (proximal pole), healing can be more difficult. These areas of the scaphoid do not have a very good blood supply. If your doctor treats this type of fracture with a cast, the cast may include the thumb and extend above the elbow to help stabilize the fracture
Bone stimulator. In some cases, your doctor may recommend the use of a bone stimulator to assist in fracture healing. This small device delivers low-intensity ultrasonic or pulsed electromagnetic waves that stimulate healing.
Surgical Treatment
If your scaphoid is broken at the waist or proximal pole or if pieces of bone are displaced, your doctor may recommend surgery. The goal of surgery is to realign and stabilize the fracture, giving it a better chance to heal.
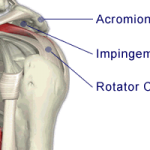
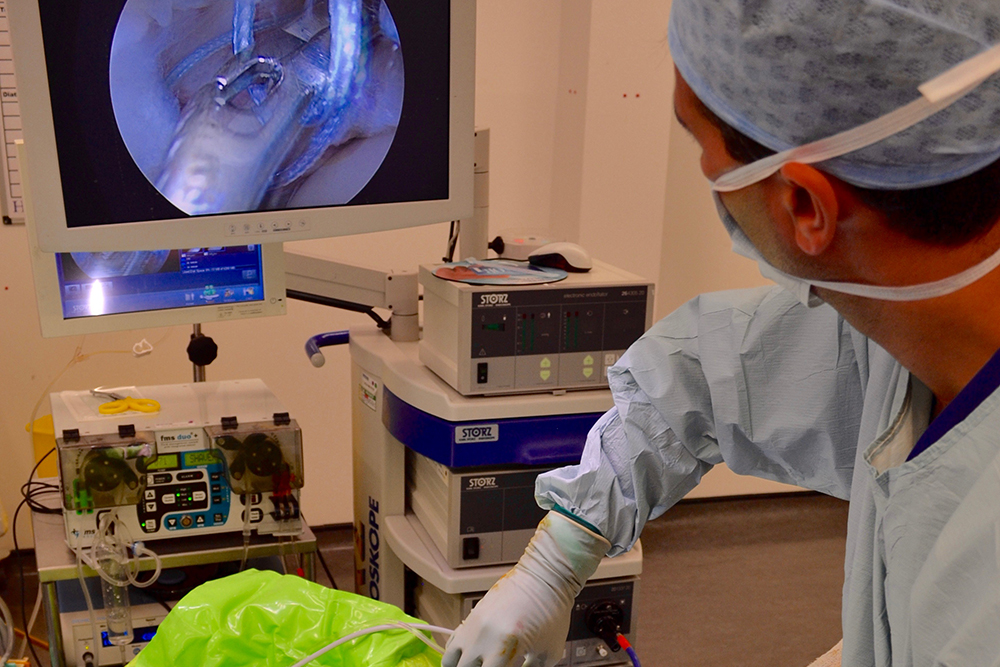
Reduction. During this procedure, your doctor will administer an anesthetic or anesthesia and manipulate the bone back into its proper position. In some cases, this is done using a limited incision and special guided instruments. In other cases, it is performed through an open incision with direct manipulation of the fracture. For some fractures, your doctor may use a tiny camera called an “arthroscope” to aid in the reduction.
Internal fixation. During this procedure, metal implants—including screws and/or wires—are used to hold the scaphoid in place until the bone is fully healed. The location and size of the surgical incision depends on what part of the scaphoid is broken. Sometimes, the screw or wire can be placed in bone fragments with a small incision. In other cases, a larger incision is needed to ensure that the fragments of the scaphoid line up properly. The incision may be made on either the front or the back of your wrist.
Bone graft. In some cases, a bone graft may be used with or without internal fixation. A bone graft is new bone that is placed around the broken bone. It can stimulate bone production and healing. The graft may be taken from your forearm bone in the same arm or from your hip.
What is the outcome
Whether your treatment is surgical or nonsurgical, you may be required to wear a cast or splint for up to 6 months or until your fracture has healed. Unlike most other fractures, scaphoid fractures tend to heal slowly. During this time, unless advanced activity is approved by your doctor, you should avoid the following activities:
Lifting, carrying, pushing, or pulling more than one pound of weight
Throwing with your injured arm
Participating in contact sports
Climbing ladders or trees
Participating in activities with a risk of falling onto your hand, such as inline skating or jumping on a trampoline
Using heavy or vibratory machinery
Smoking (which can delay or prevent fracture healing)
Some patients have wrist stiffness after scaphoid fractures. This is more common in patients who wear a cast for a long time or require more extensive surgery.
It is important to maintain full finger motion throughout your recovery period. Your doctor will provide an exercise program, and may refer you to a trained hand therapist who will help you regain as much range of motion and strength in your wrist as possible.
Despite hand therapy and a great deal of effort by the patient during home therapy, some patients may not recover the same range of motion and strength that they had before their injury.